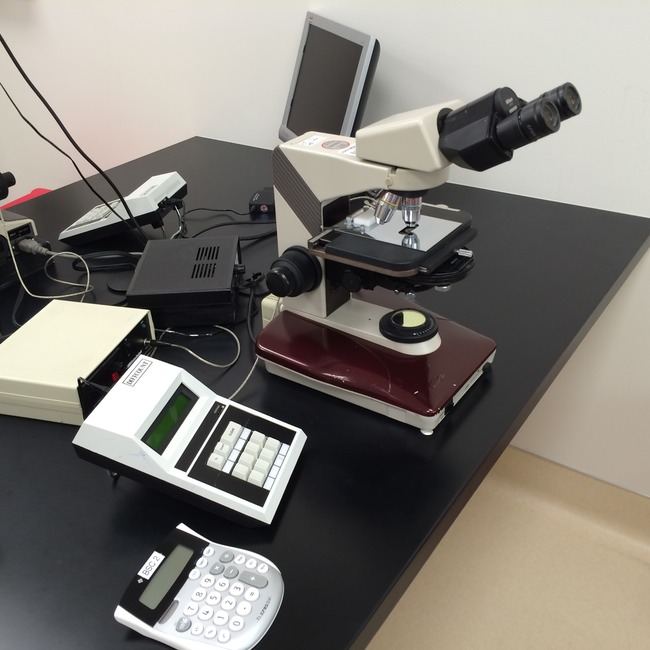
Semen Analysis (SA). The standard test of male fertility. It measures the ability to produce sufficient numbers of motile, structurally normal sperm. The main component tests of an SA are sperm count, motility, morphology, and a white blood cell differential (performed as a reflexive test if more than 1 million round cells per mL are present). A Live/Dead Viability test is performed if fewer than 25% of sperm are motile. We pay special attention to % progressively motility and % rapid & linear motility (performed by computer analysis). We calculate Total Progressively Motile Sperm per ejaculate, which is the best predictor of pregnancy.
Our reference ranges are based on the World Health Organization’s 2021 (6th ed.) recommendations, and on decades of experience with our own patients.
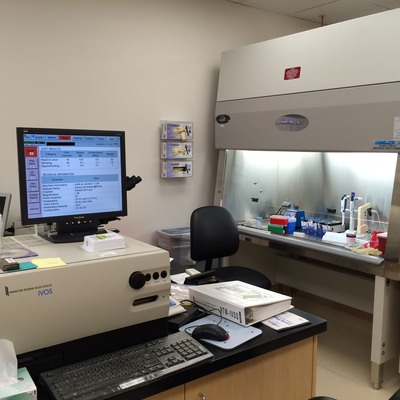
Motility Analysis by Computer: Sperm kinematics in semen, or during capacitation and hyperactivation. Poor sperm motility may be improved by Motility Enhancement. Computer-assisted sperm analysis (CASA) provides objective measures of sperm function not available by manual methods. CASA is performed in only a small proportion of labs across the country.
Post Vasectomy Check or Post Vasectomy Semen Analysis (PVSA): Presence or absence of sperm and their motility is carefully evaluated before and after centrifuging the semen.
Retrograde Urine or Post-Ejaculatory Urine Analysis: Semen analysis plus examination of the post-ejaculatory urine (PEU) to determine if sperm are present in the bladder. Sperm motility and total sperm recovered from the urine are calculated. Urine pH and osmolality are measured, since these can affect sperm viability. Recovery of functioning sperm from the bladder in cases of Retrograde Ejaculation requires careful planning of fluid intake and alkalization, or possible placement of culture medium into the bladder.
A note on Reference Ranges: As oppossed to “Normal Values”, where a clear distinction can be made between Normal and Abnormal (Pathological), a Reference Range refers to the results of a study, preferably a large multi-center trial, in which measures are made of a defined population such as couples able or not able to achieve a pregnancy in a specified time. Most of our Reference Ranges refer to the World Health Organization 2021 publication, in which the values represent the upper 95% of measures obtained from couples who became pregnant during the study. Thus, a result that is below the Reference Range means that only 5% of the pregnant couples had a similar result.