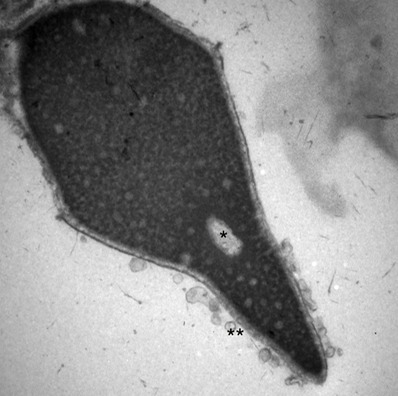
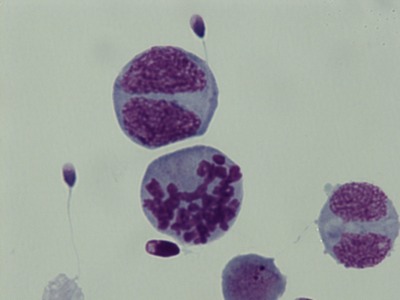
The immune system recognizes spermatozoa as “foreign” cells, since they were not present just after birth when “self” vs “not-self” was set up for each person. Usually, this is not a problem since sperm are mostly isolated from immune surveillance. However, during vasectomy, some leakage of sperm is not preventable, and the immune system starts making anti-sperm antibodies. This can also occur after trauma, and for unknown reasons. Anti-sperm antibodies may block important surface proteins and prevent fertilization. Sometimes, they make sperm stick together (agglutinate) in particular patterns such as “head-to-head” or “tail-to-tail”, but visible agglutination does not detect all cases of antibodies. Women may also develop antibodies to their partner’s sperm. Methods for detecting antibodies are fairly simple. However, there is little that can be done to prevent their effects, other than IVF with ICSI.
Almost all men with a vasectomy have antibodies to sperm, and these typically disappear after vasectomy reversal. If they don’t, this could indicate a continued leakage of sperm out of the vas, or a reason for failure to have a pregnancy.
ASSAYS: DIRECT and INDIRECT ANTI-SPERM ANTIBODIES
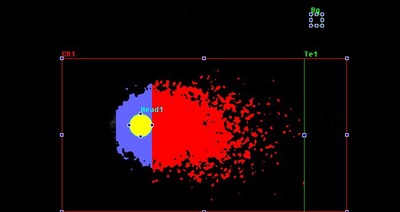
Antibodies can be detected on the male partner’s sperm by the Direct Antibody Test. This is the most reliable test. We use small beads which bind to either IgG or IgA antibodies, and record the percentage of sperm with bound beads, the location(s) of the beads (head, tail, both), and the type of antibodies.
If the partner’s sperm are not available, are too few in number, or have very poor motility, or if we are looking for anti-sperm antibodies in the woman, we can perform an Indirect Antibody Test. Here, either control donor sperm or the patient's sperm are incubated with blood plasma from the patient or wife, or seminal plasma from the male patient to allow any antibodies to bind the sperm. The sperm are washed, and the bound antibodies detected with beads as in the Direct assay.