Welcome to The UW Shoulder Site @ uwshoulder.com
Please note that information on this site was NOT authored by Dr. Frederic A Matsen III and has not been proofread or intended for general public use. Information was intended for internal use only and is a compilation for random notes and resources.
If you are looking for medical information about the treatment of shoulders, please visit shoulderarthritis.blogspot.com for an index of the many blog entries by Dr. Frederick A Matsen III.
Da Book
Standard Operating Procedures and Notes for the Shoulder Team
Joint Replacement Prophylaxis Standard Operating Procedure (SOP)
All patients who receive and arthroplasty from the Shoulder and Elbow team are advised to take antibiotics prior to any procedure that may cause bacteremia. These procedures include dental work, sigmoidoscopy, proctoscopy, cystoscopy, or pretty much any procedure with the respiratory, digestive or urinary tract.
Patients should not have any procedures that may cause bacteremia for 2 weeks prior and 3 months post any arthroplasty surgery.
Dental Procedures
Members of the Arthritis Team (Shoulder, Elbow, Hip and Knees) should feel free to prescribe prophylactic antibiotics for joint replacement patients prior to a dental procedure. For dental procedures we follow the ADA and AAOS recommendations for antibiotics but extend use of them for life (as opposed to two years following arthroplasty and for high risk patients).
Respiratory, Digestive and Urinary Tract procedures
Since some of the choices for antibiotic include vancomycin and/or gentamicin, we reserve prescribing of these antibiotics to the surgeon doing the procedure - so that they can work up and follow the patient. If there are questions as what antibiotic course to take, we can give information about the AHA's recommendations for endocarditis prophylaxis and the AAOS' recommendations listed/linked below. It is also important to note that we consider all of our patients at high risk and recommend treatment for life, compared to the common practice of only provide prophylactic treatment for two years following arthroplasty surgery.
Dental Antibiotic Prophylaxis as per the ADA recommendations:
J Am Dent Assoc, Vol 134, No 7, 895-898.
Antibiotic prophylaxis for dental patients with total joint replacements
American Dental Association; American Academy of Orthopedic Surgeons.
AHA Procedures for which endocarditis prophylaxis is recommended
Respiratory tract
Tonsillectomy and/or adenoidectomy
Surgical operations that involve respiratory mucosa
Bronchoscopy with a rigid bronchoscope
Gastrointestinal tract
Sclerotherapy for esophageal varices
Esophageal stricture dilation
Endoscopic retrograde cholangiography with biliary obstructionBiliary tract surgery
Surgical operations that involve intestinal mucosa
Genitourinary tract
Prostatic surgery
Cystoscopy
Urethral dilation
Prophylactic Regimens for Dental, Oral, Respiratory Tract, or Esophageal Procedures. (Follow-up dose no longer recommended.) Total children’s dose should not exceed adult dose.
I. Standard general prophylaxis for patients at risk:
Amoxicillin: Adults, 2.0 g (children, 50 mg/kg) given orally one hour before procedure.
II. Unable to take oral medications:
Ampicillin: Adults, 2.0 g (children 50 mg/kg) given IM or IV within 30 minutes before procedure.
III. Amoxicillin/ampicillin/penicillin allergic patients:
Clindamycin: Adults, 600 mg (children 20 mg/kg) given orally one hour before procedure. -OR-
Cephalexin* or Cefadroxil*: Adults, 2.0 g (children 50 mg/kg) orally one hour before procedure. -OR-
Azithromycin or Clarithromycin: Adults, 500 mg (children 15 mg/kg) orally one hour before procedure.
IV. Amoxicillin/ampicillin/penicillin allergic patients unable to take oral medications:
Clindamycin: Adults, 600 mg (children 20 mg/kg) IV within 30 minutes before procedure. -OR-
Cefazolin*: Adults, 1.0 g (children 25 mg/kg) IM or IV within 30 minutes before procedure.
*Cephalosporins should not be used in patients with immediate-type hypersensitivity reaction to penicillins.
Prophylactic Regimens for Genitourinary/Gastrointestinal Procedures: (Joint Replacement Patients should be considered High Risk for our purposes)
I. High-risk patients:
Ampicillin plus gentamicin: Ampicillin (adults, 2.0 g; children 50 mg/kg) plus gentamicin 1.5 mg/kg (for both adults and children, not to exceed 120 mg) IM or IV within 30 minutes before starting procedure. 6 hours later, ampicillin (adults, 1.0 g; children, 25 mg/kg) IM or IV, or amoxicillin (adults, 1.0 g; children, 25 mg/kg) orally.
II. High-risk patients allergic to ampicillin/amoxicillin:
Vancomycin plus gentamicin: Vancomycin (adults, 1.0 g; children, 20 mg/kg) IV over 1–2 hours plus gentamicin 1.5 mg/kg (for both adults and children, not to exceed 120 mg) IM or IV. Complete injection/infusion within 30 minutes before starting procedure.
III. Moderate-risk patients:
Amoxicillin: Adults, 2.0 g (children 50 mg/kg) orally one hour before procedure -OR-
Ampicillin: Adults, 2.0 g (children 50 mg/kg) IM or IV within 30 minutes before starting procedure.
IV. Moderate-risk patients allergic to ampicillin/amoxicillin:
Vancomycin: Adults, 1.0 g (children 20 mg/kg) IV over 1–2 hours. Complete infusion within 30 minutes of starting the procedure.
JAMA. 1997 Jun 11;277(22):1794-801
Prevention of bacterial endocarditis. Recommendations by the American Heart Association.
Dajani AS, Taubert KA, Wilson W, Bolger AF, Bayer A, Ferrieri P, Gewitz MH, Shulman ST, Nouri S, Newburger JW, Hutto C, Pallasch TJ, Gage TW, Levison ME, Peter G, Zuccaro G Jr.
AAOS Antibiotic Prophylaxis for Bacteremia in Patients with Joint Replacements
Antibiotic Prophylaxis for Bacteremia in Patients with Joint Replacements
This Information Statement was developed as an educational tool based on the opinion of the authors. Readers are encouraged to consider the information presented and reach their own conclusions.
More than 1,000,000 total joint arthroplasties are performed annually in the United States, of which approximately 7 percent are revision procedures.1 Deep infections of total joint replacements usually result in failure of the initial operation and the need for extensive revision, treatment and cost. Due to the use of perioperative antibiotic prophylaxis and other technical advances, deep infection occurring in the immediate postoperative period resulting from intraoperative contamination has been markedly reduced in the past 20 years.
Bacteremia from a variety of sources can cause hematogenous seeding of bacteria onto joint implants, both in the early postoperative period and for many years following implantation.2 In addition, bacteremia may occur in the course of normal daily life3-5 and concurrently with dental, urologic and other surgical and medical procedures.5 The analogy of late prosthetic joint infections with infective endocarditis is invalid as the anatomy, blood supply, microorganisms and mechanisms of infection are all different.6
It is likely that bacteremia associated with acute infection in the oral cavity,7,8 skin, respiratory, gastrointestinal and urogenital systems and/or other sites can and do cause late implant infection.8 Practitioners should maintain a high index of suspicion for any change or unusual signs and symptoms (e.g. pain, swelling, fever, joint warm to touch) in patients with total joint prostheses. Any patient with an acute prosthetic joint infection should be vigorously treated with elimination of the source of the infection and appropriate therapeutic antibiotics.8,9
Patients with joint replacements who are having invasive procedures or who have other infections are at increased risk of hematogenous seeding of their prosthesis. Antibiotic prophylaxis may be considered, for those patients who have had previous prosthetic joint infections, and for those with other conditions that may predispose the patient to infection (Table 1). 8,10-16 There is evidence that some immunocompromised patients with total joint replacements may be at higher risk for hematogenous infections.10-18 However, patients with pins, plates and screws, or other orthopaedic hardware that is not within a synovial joint are not at increased risk for hematogenous seeding by microorganisms.
Given the potential adverse outcomes and cost of treating an infected joint replacement, the AAOS recommends that clinicians consider antibiotic prophylaxis for all total joint replacement patients prior to any invasive procedure that may cause bacteremia. This is particularly important for those patients with one or more of the following risk factors.
Table 1. Patients at Potential Increased Risk of Hematogenous Total Joint Infection8,10-16,18
- All patients with prosthetic joint replacement.
- Immunocompromised/immunosuppressed patients
- Inflammatory arthropathies (e.g.: rheumatoid arthritis, systemic lupus erythematosus)
- Drug-induced immunosuppression
- Radiation-induced immunosuppression
- Patients with co-morbidities (e.g.: diabetes, obesity, HIV, smoking)
- Previous prosthetic joint infections
- Malnourishment
- Hemophilia
- HIV infection
- Insulin-dependent (Type 1) diabetes
- Malignancy
- Megaprostheses
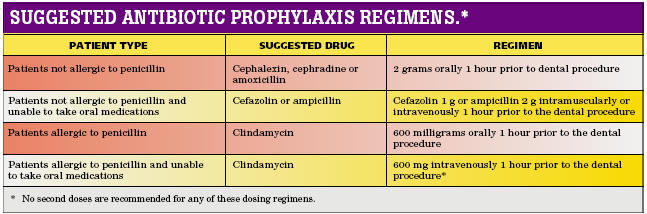
Prophylactic antibiotics prior to any procedure that may cause bacteremia are chosen on the basis of its activity against endogenous flora that would likely to be encountered from any secondary other source of bacteremia, its toxicity, and its cost. In order to prevent bacteremia, an appropriate dose of a prophylactic antibiotic should be given prior to the procedure so that an effective tissue concentration is present at the time of instrumentation or incision in order to protect the patient’s prosthetic joint from a bacteremia induced periprosthetic sepsis. Current prophylactic antibiotic recommendations for these different procedures are listed in Table 2. 19
Occasionally, a patient with a joint prosthesis may present to a given clinician with a recommendation from his/her orthopaedic surgeon that is not consistent with these recommendations. This could be due to lack of familiarity with the recommendations or to special considerations about the patient's medical condition which are not known to either the clinician or orthopaedic surgeon. In this situation, the clinician is encouraged to consult with the orthopaedic surgeon to determine if there are any special considerations that might affect the clinician’s decision on whether or not to pre-medicate, and may wish to share a copy of these recommendations with the physician, if appropriate. After this consultation, the clinician may decide to follow the orthopaedic surgeon’s recommendation, or, if in the clinician’s professional judgment, antibiotic prophylaxis is not indicated, may decide to proceed without antibiotic prophylaxis.
Table 2
Procedure Antimicrobial Agent Dose Timing Duration Dental Cephalexin, cephradine, amoxicillin 2 gm PO 1 hour prior to procedure Discontinued within 24 hours of the procedure. For most outpatient/office-based procedures a single pre-procedure dose is sufficient. Ophthalmic Gentamicin, tobramycin, ciprofloxacin, gatifloxacin, levofloxacin, moxifloxacin, ofloxacin, or meomycin-gramicidin-polymyxin B cefazolin Multiple drops topically over 2 to 24 hours or 100 mg subconjunctivally Consult ophthalmologist or pharmacist for dosing regimen Orthopaedic† CefazolinCefuroxime OR Vancomycin 1-2 g IV
1.5 g IV
1 g IVBegin dose 60
minutes prior to
procedureVascular Cefazolin OR
Vancomyin1-2 g IV
1 g IVBegin dose 60 minutes prior to procedure Gastrointestinal Esophageal, gastroduodenal
Cefazolin 1-2 g IV Begin dose 60 minutes prior to procedure Biliary tract Cefazolin 1-2 g IV Colorectal Neomycin + erythromycin base (oral) 1 g Dependent on time of procedure, consult with GI physician and/or pharmacist OR metronidazole (oral) 1 g Head and neck Clindamycin + gentamicin OR
cefazolin600-900 mg IV
1.5 mg/kg IV
1-2 g IVBegin dose 60 minutes prior to procedure Obstetric and gynecological Cefoxitin, cefazolin
Ampicillin/sulbactam1-2 g IV
3 g IVBegin dose 60 minutes prior to procedure Genitourinary Ciprofloxacin 500 mg PO or
400 mg IV1 hour prior to procedure
Begin dose 60 minutes prior to procedure
† If a tourniquet is used the entire dose of antibiotic must be infused prior to its inflation
This statement provides recommendations to supplement practitioners in their clinical judgment regarding antibiotic prophylaxis for patients with a joint prosthesis. It is not intended as the standard of care nor as a substitute for clinical judgment as it is impossible to make recommendations for all conceivable clinical situations in which bacteremias may occur. The treating clinician is ultimately responsible for making treatment recommendations for his/her patients based on the clinician’s professional judgment.
Any perceived potential benefit of antibiotic prophylaxis must be weighed against the known risks of antibiotic toxicity, allergy, and development, selection and transmission of microbial resistance. Practitioners must exercise their own clinical judgment in determining whether or not antibiotic prophylaxis is appropriate.
References:
- Number of Patients, Number of Procedures, Average Patient Age, Average Length of Stay - National Hospital Discharge Survey 1998-2005. Data obtained from: U.S. Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Health Statistics.
- Rubin R, Salvati EA, Lewis R: Infected total hip replacement after dental procedures. Oral Surg. 1976;41:13-23.
- Bender IB, Naidorf IJ, Garvey GJ: Bacterial endocarditis: A consideration for physicians and dentists. J Amer Dent Assoc 1984;109:415-420.
- Everett ED, Hirschmann JV: Transient bacteremia and endocarditis prophylaxis: A review. Medicine 1977; 56:61-77.
- Guntheroth WG: How important are dental procedures as a cause of infective endocarditis? Amer J Cardiol 1984;54:797-801.
- McGowan DA: Dentistry and endocarditis. Br Dent J 1990;169:69.
- Bartzokas CA, Johnson R, Jane M, Martin MV, Pearce PK, Saw Y: Relation between mouth and haematogenous infections in total joint replacement. BMJ 1994;309:506-508.
- Ching DW, Gould IM, Rennie JA, Gibson PH: Prevention of late haematogenous infection in major prosthetic joints. J Antimicrob Chemother 1989;23:676-680.
- Pallasch TJ, Slots J: Antibiotic prophylaxis and the medically compromised patient. Periodontology 2000 1996;10:107-138
- Rubin R, Salvati EA, Lewis R: Infected total hip replacement after dental procedures. Oral Surg. 1976;41:13-23.
- Brause BD: Infections associated with prosthetic joints. Clin Rheum Dis 1986;12:523-536.
- Jacobson JJ, Millard HD, Plezia R, Blankenship JR: Dental treatment and late prosthetic joint infections. Oral Surg Oral Med Oral Pathol 1986; 61:413-417.
- Johnson DP, Bannister GG: The outcome of infected arthroplasty of the knee. J Bone Joint Surg; 688:289-291.
- Jacobson JJ, Patel B, Asher G, Wooliscroft JO, Schaberg D: Oral Staphyloccus in elderly subjects with rheumatiod arthritis. J Amer Geriatr Soc 1997;45:1-5.
- Murray RP, Bourne WH, Fitzgerald RH: Metachronus infection in patients who have had more than one total joint arthroplasty. J Bone Joint Surg 1991;73-A:1469-1474.
- Poss R, Thornhill TS, Ewald FC, Thomas WH, Batte NJ, Sledge CB: Factors influencing the incidence and outcome of infection following total joint arthroplasty. Clin Orthop 1984;182:117-126.
- Council on Dental Therapeutics. Management of dental patients with prosthetic joints. J Amer Dent Assoc 1990;121:537-538.
- Berbari EF, Hanssen AD, Duffy MC, Ilstrup DM, Harmsen WS, Osmon DR: Risk factors for prosthetic joint infection: case-control study. Clin Infectious Dis 1998; 27:1247-1254.
- Antibiotic Prophylaxis for Surgery. The Medical Letter 2006; 4 (52): 83-88.
Information Statement 1033
AAOS Antibiotic Prophylaxis for Urological Patients with Total Joint Replacements 2002 - (These are the old recomendations)
Risk Stratification of Bacteremic Urologic Procedures
- Any stone manipulation (includes shock wave lithotripsy)
- Any procedure with transmural incision into urinary tract (does not include simple ligation with excision or percutaneous drainage procedure)
- Any endoscopic procedures of upper tract (ureter and kidney)
- Any procedure that includes bowel segments
- Transrectal prostate biopsy
- Any procedure with entry into the urinary tract (except for transurethral catheterization) in individuals with higher risk of bacterial colonization:
- Indwelling catheter or intermittent catheterization
- Indwelling ureteral stent
- Urinary retention
- History of recent / recurrent urinary tract infection or prostatitis
- Urinary diversion
Lower Risk**
- Endoscopic procedures into urethra and bladder without stone manipulation or incision (includes fulguration and mucosal biopsy, if no incision)
- Open surgical or laparoscopic procedures without stone manipulation or incision into the urinary tract
- Catheterization for drainage or diagnostic instrumentation, including both transurethral and percutaneous access
* Prophylaxis for higher risk patients should be considered for patients with total joint replacement that meet the criteria in Table 1. No other patients should be considered for antibiotic prophylaxis prior to urologic procedures on the basis of the orthopaedic implant alone, although antibiotics still may be indicated for prophylaxis against urinary tract or other infections.
** Prophylaxis for lower risk patients not indicated on the basis of the orthopaedic implant alone, although antibiotics still may be indicated for prophylaxis against urinary tract or other infections.
Suggested Antibiotic Prophylaxis Regimens
A prophylactic antibiotic is chosen on the basis of its activity against endogenous flora likely to be encountered, its toxicity, and its cost. In order to prevent bacteriuria, an appropriate dose of a prophylactic antibiotic should be given preoperatively so that effective tissue concentration is present at the time of instrumentation or incision.
- Recommended agents include
- A single systemic level dose of a quinolone (e.g., ciprofloxacin, 500 mg; levofloxacin, 500 mg; ofloxacin, 400 mg) orally one to two hours preoperatively.
- Ampicillin 2 gm IV (or Vancomycin 1 gm IV over 1 to 2 hours, in patients allergic to ampicillin) plus Gentamicin 1.5 mg/kg IV 30 to 60 minutes preoperatively.9
- For some procedures, additional or alternative agents may be considered for prophylaxis against specific organisms.
Also see AAOS Antibiotic Prophylaxis for Dental Patients with Total Joint Replacements
- Bartzokas CA, Johnson R, Jane M, Martin MV, Pearce PK, Saw Y: Relation between mouth and haematogenous infections in total joint replacement. BMJ 1994;309:506-508.
- Bender IB, Naidorf IJ, Garvey GJ: Bacterial endocarditis: A consideration for physicians and dentists. J Amer Dent Assoc 1984;109:415-420.
- Berbari EF, Hanssen AD, Duffy MC, Ilstrup DM, Harmsen WS, Osmon DR: Risk factors for prosthetic joint infection: case-control study. Clin Infectious Dis 1998; 27:1247-1254.
- Brause BD: Infections associated with prosthetic joints. Clin Rheum Dis 1986;12:523-536.
- Ching DW, Gould IM, Rennie JA, Gibson PH: Prevention of late haematogenous infection in major prosthetic joints. J Antimicrob Chemother 1989;23:676-680.
- Chodak GW and Plaut ME: Systemic antibiotics for prophylaxis in urologic surgery: a critical review. J. Urology 1979; 121: 695-699.
- Christiano AP, Hollowell CMP, Kim H, Kim J, Patel R, Bales GT, Gerber GS: Double-blind randomized comparison of single-dose ciprofloxacin versus intravenous cefazolin in patients undergoing outpatient endourologic surgery. Urology 2000; 55: 182-185.
- Cundiff GW, McLennan, MT, Bent, AE: Randomized trial of antibiotic prophylaxis for combined urodynamics and cystourethroscopy. Obstetrics & Gynecology 1999; 93: 749-752.
- Dajani AS. Taubert KA. Wilson W. Bolger AF. Bayer A. Ferrieri P. Gewitz MH. Shulman ST. Nouri S. Newburger JW. Hutto C. Pallasch TJ. Gage TW. Levison ME. Peter G. Zuccaro G Jr. Prevention of bacterial endocarditis. Recommendations by the American Heart Association. JAMA. 1997; 277:1794-1801.
- Everett ED, Hirschmann JV: Transient bacteremia and endocarditis prophylaxis: A review. Medicine 1977; 56:61-77.
- Grabe M: Perioperative antibiotic prophylaxis in urology. Current Opinion in Urology 2001; 11: 81-85.
- Guntheroth WG: How important are dental procedures as a cause of infective endocarditis? Amer J Cardiol 1984;54:797-801.
- Hanssen AD, Osmon DR, Nelson CL: Prevention of deep prosthetic joint infection. J Bone Joint Surg 1996;78-A(3):458-471.
- Jacobson JJ, Millard HD, Plezia R, Blankenship JR: Dental treatment and late prosthetic joint infections. Oral Surg Oral Med Oral Pathol 1986; 61:413-417.
- Jacobson JJ, Patel B, Asher G, Wooliscroft JO, Schaberg D: Oral Staphyloccus in elderly subjects with rheumatiod arthritis. J Amer Geriatr Soc 1997;45:1-5.
- Johnson DP, Bannister GG: The outcome of infected arthroplasty of the knee. J Bone Joint Surg 1986;688:289-291.
- Kapoor DA, Klimberg IW, Malek GH, Wegenke JD, Cox CE, Patterson AL, Graham E, Echols RM, Whalen E and Kowalsky SF: Single-dose ciprofloxacin versus placebo for prophylaxis during transrectal prostate biopsy. Urology 1998; 52: 552-558.
- Kraklau DM and Wolf JS, Jr.: Review of antibiotic prophylaxis recommendations for office-based urologic procedures. Techniques in Urology 1999; 5: 123-128.
- Larsen EH, Gasser TC and Madsen PO: Antimicrobial prophylaxis in urologic surgery. Urological Clinics of North America 1986; 13: 591-604.
- Murray RP, Bourne WH, Fitzgerald RH: Metachronus infection in patients who have had more than one total joint arthroplasty. J Bone Joint Surg 1991;73-A:1469-1474.
- Naber KG, Hofstetter AG, Bruhl P, Bichler K-H, Lebert C: Guidelines for the perioperative prophylaxis in urological interventions of the urinary and male genital tract. Int J Antimicrobial Agents 2001; 17: 321-326.
- Olson E, Cookson B: Do antimicrobials have a role in preventing septicaemia following instrumentation of the urinary tract? Journal of Hospital Infection 2000: 85-97.
- Pallasch TJ, Slots J: Antibiotic prophylaxis and the medically compromised patient. Periodontology 2000 1996;10:107-138
- Pearle MS and Roehrborn CG: Antimicrobial prophylaxis prior to shock wave lithotripsy in patients with sterile urine before treatment: a meta-analysis and cost-effectiveness analysis. Urology 1997; 49: 679-686.
- Poss R, Thornhill TS, Ewald FC, Thomas WH, Batte NJ, Sledge CB: Factors influencing the incidence and outcome of infection following total joint arthroplasty. Clin Orthop 1984;182:117-126.
- Rubin R, Salvati EA, Lewis R: Infected total hip replacement after dental procedures. Oral Surg. 1976;41:13-23.
- Scholz M, Luftenegger W, Harmuth H, Wolf D and Holtl W: Single-dose antibiotic prophylaxis in transurethral resection of the prostate: a prospective randomized trial. Br. J. Urology 1998; 81: 827-829.
- Terris MK: Recommendations for prophylactic antibiotic use in genitourinary surgery. Contemporary Urology Sept 2001; 12-27.
- Pallasch TJ, Slots J: Antibiotic prophylaxis and the medically compromised patient. Periodontology 2000 1996;10:107-138
- Rubin R, Salvati EA, Lewis R: Infected total hip replacement after dental procedures. Oral Surg. 1976;41:13-23.
- Hanssen AD, Osmon DR, Nelson CL: Prevention of deep prosthetic joint infection. J Bone Joint Surg 1996;78-A(3):458-471.
- Bender IB, Naidorf IJ, Garvey GJ: Bacterial endocarditis: A consideration for physicians and dentists. J Amer Dent Assoc 1984;109:415-420.
- Everett ED, Hirschmann JV: Transient bacteremia and endocarditis prophylaxis: A review. Medicine 1977; 56:61-77.
- Guntheroth WG: How important are dental procedures as a cause of infective endocarditis? Amer J Cardiol 1984;54:797-801.
- Jacobson JJ, Schweitzer SO, DePorter DJ, Lee JJ: Antibiotic prophylaxis for dental patients with joint prostheses? A decision analysis. Int J Technol Assess Health Care 1990;6:569-587.
- Tsevat J, Durand-Zaleski I, Pauker SG: Cost-effectiveness of antibiotic prophylaxis for dental procedures in patients with artificial joints. Amer J Pub Health 1989;79:739-743.
- Norden CW: Prevention of bone and joint infections. Amer J Med 1985;78(Suppl 6B):229-232.
- McGowan DA: Dentistry and endocarditis. Br Dent J 1990;169:69.
- Bartzokas CA, Johnson R, Jane M, Martin MV, Pearce PK, Saw Y: Relation between mouth and haematogenous infections in total joint replacement. BMJ 1994;309:506-508.
- Ching DW, Gould IM, Rennie JA, Gibson PH: Prevention of late haematogenous infection in major prosthetic joints. J Antimicrob Chemother 1989;23:676-680.
- Council on Dental Therapeutics. Management of dental patients with prosthetic joints. J Amer Dent Assoc 1990;121:537-538.
- Eskinazi D, Rathburn W: Is systematic antimicrobial prophylaxis justified in dental patients with prosthetic joints? Oral Surg Oral Med Oral Pathol 1988;66:430-431.
- Cawson RA: Antibiotic prophylaxis for dental treatment: For hearts but not for prosthetic joints. Br Dent J 1992;304:933-934.
- Brause BD: Infections associated with prosthetic joints. Clin Rheum Dis 1986;12:523-536.
- Murray RP, Bourne WH, Fitzgerald RH: Metachronus infection in patients who have had more than one total joint arthroplasty. J Bone Joint Surg 1991;73-A:1469-1474.
- Poss R, Thornhill TS, Ewald FC, Thomas WH, Batte NJ, Sledge CB: Factors influencing the incidence and outcome of infection following total joint arthroplasty. Clin Orthop 1984;182:117-126.
- Jacobson JJ, Millard HD, Plezia R, Blankenship JR: Dental treatment and late prosthetic joint infections. Oral Surg Oral Med Oral Pathol 1986; 61:413-417.
- Johnson DP, Bannister GG: The outcome of infected arthroplasty of the knee. J Bone Joint Surg 1986;688:289-291.
- Jacobson JJ, Patel B, Asher G, Wooliscroft JO, Schaberg D: Oral Staphyloccus in elderly subjects with rheumatiod arthritis. J Amer Geriatr Soc 1997;45:1-5.
- Berbari EF, Hanssen AD, Duffy MC, Ilstrup DM, Harmsen WS, Osmon DR: Risk factors for prosthetic joint infection: case-control study. Clin Infectious Dis 1998; 27:1247-1254.
- Dajani AS, Taubert KA, Wilson W, Bolger AF, Bayer A, Ferrieri P, Gewitz MH, Shulman ST, Nouri S, Newburger JW, Hutto C, Pallasch TJ, Gage TW, Levison ME, Peter G, Zuccaro G: Prevention of bacterial endocarditis: Recommendations by the American Heart Association. From the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young. JAMA 1997;277:1974-1801.